Scleroderma is an immune-mediated disease of the connective tissue, characterized by fibrosis of the skin and underlying organs, it has the highest mortality rate of any rheumatologic disorder, there is no cure, and only limited targeted treatments. We propose that T cell interactions with structural cells of the skin such as keratinocytes and fibroblasts lie at the balance of tissue homeostasis and disease-associated pathogenesis.
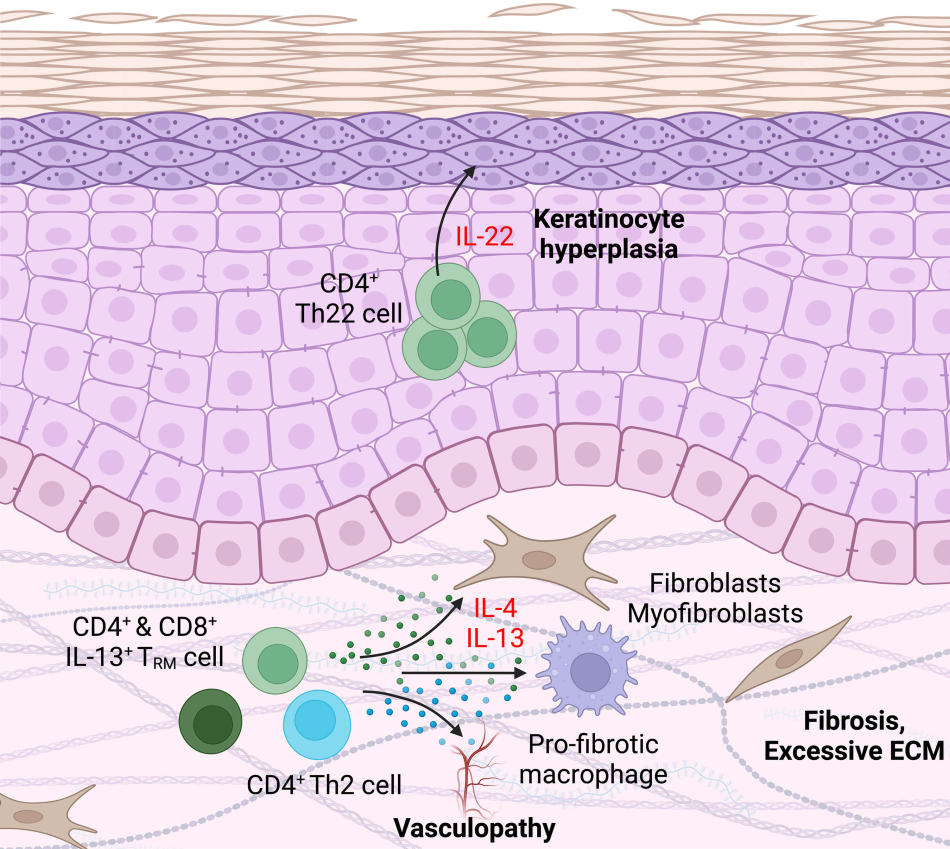
T cells have an essential role in fibroblast dysregulation leading to tissue destruction in scleroderma, but major questions remain unanswered including:
- Which specific disease-associated T cell and fibroblast populations interact within affected patient skin?
- Are the T cell cytokines implicated in disease (IL-13, IL-4, etc.) directly responsible for transcriptional and functional dysregulation of scleroderma-associated fibroblasts?
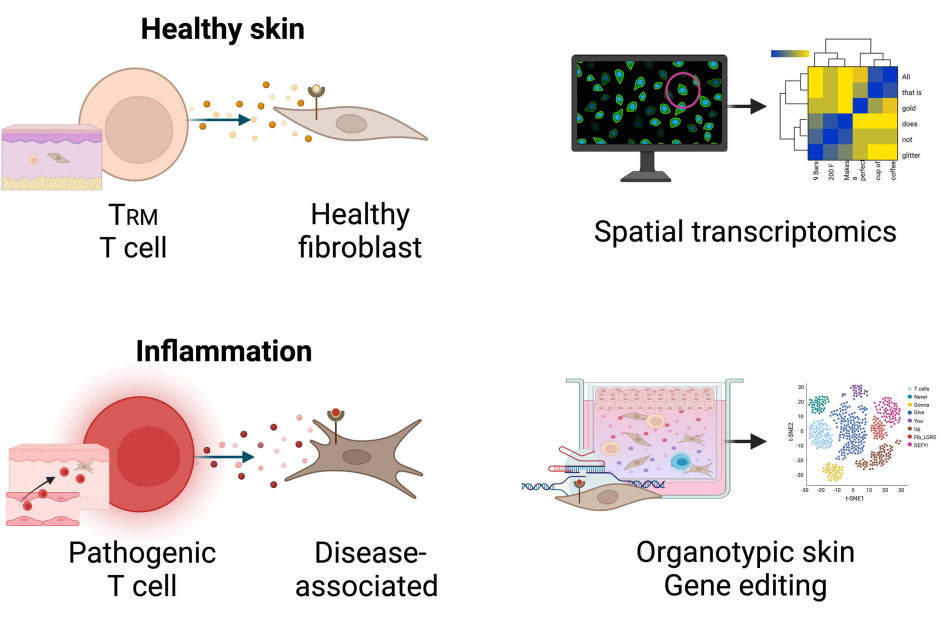
Project schematic
a. We hypothesize that in healthy skin, resident-memory T cells support homeostatic fibroblast subset stability, which is disrupted by pathogenic T cell cytokine activity during scleroderma.
b. Our ongoing studies use innovative techniques including spatial genomics, organotypic 3D skin culture models, and gene editing to fill critical knowledge gaps about T cells during disease and overcome existing technical hurdles in the field to inform future therapeutics for scleroderma.


