
What Should I Eat? Understanding the Relationship Between Diet and IBD
Recently diagnosed inflammatory bowel disease (IBD) patients often ask: did a certain food cause my disease, and can another food cure it? While no single diet can cure or cause IBD, diet can be an important factor for IBD patients to take into consideration as they seek ways to manage symptoms and maintain good nutrition.
IBD, which manifests as Crohn’s disease and ulcerative colitis, is an autoimmune disease that causes the immune system to attack the body’s gastrointestinal (GI) system. Symptoms might include abdominal pain, internal bleeding, and intestinal inflammation, which can make sticking to a consistent and balanced diet seem impossible.
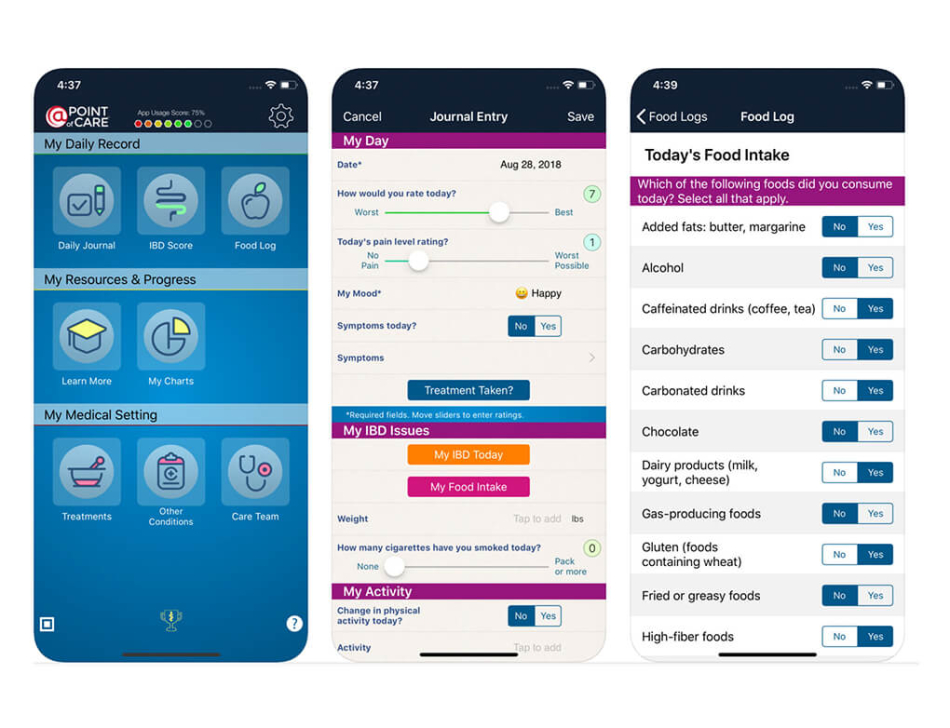
We spoke with Dr. James Lord, Virginia Mason gastroenterologist and researcher at the Benaroya Research Institute at Virginia Mason (BRI), about the relationship between diet and IBD symptoms. Dr. Lord recently helped develop the My IBD Manager app, which helps IBD patients track their symptoms against their diets, with the support of BRI, Point of Care, and the American Gastroenterological Association. Read on to hear Dr. Lord’s advice for IBD patients who are learning about diet management, and how the My IBD Manager app can help patients to understand and reduce painful symptoms caused by IBD.
How should IBD patients think about their diets?
For IBD patients, diets are a way to manage symptoms. There is little to no good data that proves dietary strategies will alter the underlying inflammation of IBD by any objective measurements; however, there are myriad anecdotal reports and case series of patients reporting fewer or less severe symptoms of IBD in response to certain dietary interventions.
This makes intuitive sense. Everyone's GI tract can be upset, at least a little, by eating certain things. When you have IBD, however, it’s like someone’s turned up the amplifier on these symptoms. Food that would normally bother a person only a little bit can trigger a host of painful symptoms including diarrhea, intestinal pain, and bloating.
How does the My IBD Manager app help manage symptoms/routines?
My IBD Manager empowers individuals to be scientists themselves so that they can study correlations between what they eat and how they feel over an extended period of time. We know that if people don't record such things carefully and only depend on memory, they can end up with a lot of selective, anecdotal associations which may not really reflect the truth. This is called "recall bias," which the app helps to reduce.
The app allows patients to carefully monitor what they eat alongside what their symptoms are from day to day. As a result, patients can keep track of what happens when they adhere to a particular dietary intervention, such as eliminating a certain food from their diet or starting a new diet.
What do you say to patients about how diet might affect their symptoms?
Unfortunately, there aren’t a lot of universal diet recommendations for IBD patients because of how much people vary in their responses to different foods. What might work great for one patient could be terrible for another. I recommend that patients pay attention to what they eat to identify correlations between certain foods and different symptoms and work with their doctors to come up with a dietary plan that works for them.
For some people, cutting out dairy and/or gluten alone can have a big effect. Others report positive results from the specific carbohydrate diet (SCD), which is similar to the paleo diet. The low FODMAPs diet is one of the most difficult diets to comply with, particularly for vegetarians, but some patients think it’s worth it. Ultimately, it’s really important for patients to balance nutrition with their dietary symptom management strategies, as some extreme diets can result in vitamin or protein malnutrition.
There is one universal recommendation for patients living with fibrostenotic Crohn's disease, which causes severe fibrotic narrowings in the small intestine. For these patients, I uniformly recommend avoiding insoluble fiber, or "roughage," such as berry seeds, peels and skins, stems, rinds, and crude pulp. Unfortunately, this can make it tricky to eat a balanced diet.
Immuno-what? Hear the latest from BRI
Keep up to date on our latest research, new clinical trials and exciting publications.


