Thanks to a three-year grant from the National Multiple Sclerosis Society, Dr. Bettelli is studying the role of TRMs in MS and how they interact with B cells.
She is in the very early stages of this research, but she has a big, bold idea at the back of her mind: Is there a way to force these MS-causing cells to leave the brain and spinal cord? If so, it could revolutionize the way we treat MS.
Using Models to Study MS
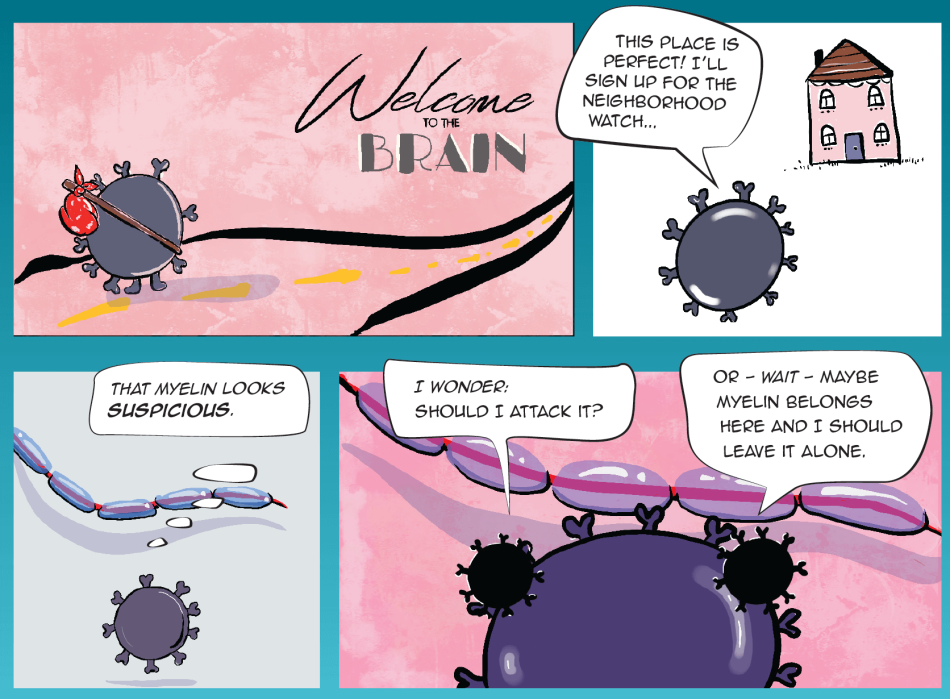
We think of TRMs as guardians in your immune system. They pick a specific tissue — say your brain or spinal cord — move in, and become residents of that tissue. They stay in that tissue, watching for harmful invaders. If they see one, unlike other immune cells that have to travel from afar via the bloodstream, these cells are available on-site and can quickly recall their first encounter with the invader and help eliminate it.
TRMs are generally considered protective and beneficial. But experts believe that in MS, some TRMs mistakenly flag a part of the body’s brain and spinal cord (the myelin sheath that surrounds and protects nerves) as an invader that needs to be attacked.
The fact that TRMs take up residence in a specific tissue has made them difficult to study. Part of the challenge of studying immune cells in the brain and spinal cord is that these tissue sites are delicate and hard to access. Taking a biopsy of this area would be too invasive and risky. And that’s why learning about TRMs in the central nervous system (CNS) is best done with models. Thankfully, Dr. Bettelli is a leading expert in building MS lab models — and the lab is her happy place.
“My favorite thing is being in the lab. I’ll take it 10 times over being in my office,” she laughs. “In the lab, my team and I have been working to create different types of models to test and manipulate TRMs in ways that we could not do otherwise.”
Dr. Bettelli has several lab tests mapped out: She and her team have built a model driven by TRMs, another driven by B cells, and another that examines both cell types together. This will enable her to study their different roles and relationships.
Her ultimate goal is to pinpoint the specific cellular markers that could be used to force both TRMs and B cells to leave the CNS — and help prevent relapse or progression of MS. The ability to do this has the potential to take MS treatments to the next level, improving the lives of the more than 2.8 million people living with the disease.
“Right now, TRMs are this black box and we don’t really understand how to eliminate those that are harmful,” Dr. Bettelli says. “I’m looking forward to learning more about them and to determine how they communicate with B cells in the context of MS.”